23.2.2021
Cardiovascular diseases (CVDs) such as coronary artery disease, cerebrovascular disease, deep vein thrombosis, etc. are structural and functional disorders of heart and blood vessels [1]. According to the World Health Organization, CVDs are the global leading cause of death, which 17.9 million people died from in 2016. This represents 31% of all global deaths and the number is expected to increase to 23.6 million by 2030. 85% of CVDs are due to heart attack and stroke, which are caused by blockage of vessels that transport blood to the heart [2]. Traditional treatment is performed by transplantation of autologous healthy blood vessel via bypassing diseased ones. However, the autologous blood vessels fail to meet the requirements for clinical applications, especially for elderly patients. Synthetic vascular grafts and tissue constructs are the most promising alternatives to the current approaches[3]. They are commercially available and composed of various biomaterials such as expanded polytetrafluoroethylene (e-PTFE), polyethylene terephthalate (PET) and polyurethane (PU), which in general do not trigger immune response or inflammation [4]. However, the vascular grafts available in the market are mostly for blood vessels in which the diameter is larger than 6 mm. These biostable synthetic materials are not ideal for smaller diameter blood vessels (SDVG) (< 6mm) due to their tendency to cause early thrombosis. Hence, one of the main focuses of vascular tissue engineering is creating tissue-engineered vascular grafts (TEVGs) which can be fabricated as a patient-specific graft in terms of disease and the organ when a small diameter vascular graft is required. It is possible to recapitulate the physiological conditions (both cellular and extracellular matrix (ECM) components) according to the body´s needs and TEVGs could lower potential immune response and increase durability while facilitating more integrated surrounding tissue.
3D printing is one of the additive manufacturing techniques, widely used in tissue engineering because of its feasibility to build complex tissue constructs and control over fabrication and cell distribution [5,6]. The main steps in the bioprinting process are; imaging and design, choice of materials and cells, and printing of the tissue construct[6]. Additionally, materials (ink) that will be used in 3D printing must have characteristics such as relatively low viscosity, printability, structural fidelity, and cell binding sites for the attachment, infiltration, and proliferation of cells [7].
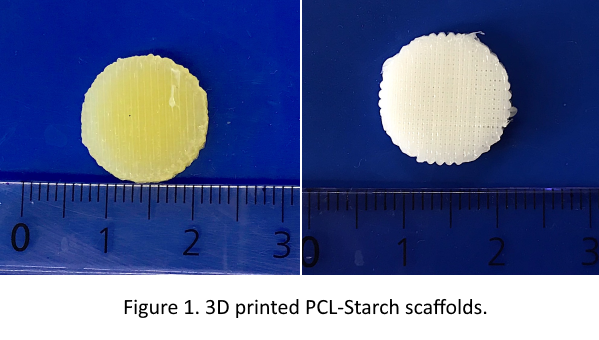
The main objective that we focus on this PhD project is to prepare mechanically stable and bioactive scaffolds, as a model system for SDVG, which will enable the growth of endothelial cells in the form of a monolayer. The first step for achieving this objective is to formulate inks that are suitable for 3D printing and to mimic the ECM in terms of chemical composition, structure, and mechanical properties. For this purpose, natural polymers like polysaccharides (PS) and glycosaminoglycans (GAGs) along with polycaprolactone is used. Amino acids and peptide are conjugated with PS/GAGs, which will increase the attachment of endothelial cells and biocompatibility of material, in general.
References
- Elomaa, L. and Y.P. Yang, Additive manufacturing of vascular grafts and vascularized tissue constructs. Tissue Engineering Part B: Reviews, 2017. 23(5): p. 436-450.
- https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
- Veith, F.J., et al., Preoperative saphenous venography in arterial reconstructive surgery of the lower extremity. Surgery, 1979. 85(3): p. 253-256.
- Radke, D., et al., Tissue Engineering at the Blood‐Contacting Surface: A Review of Challenges and Strategies in Vascular Graft Development. Advanced healthcare materials, 2018. 7(15): p. 1701461.
- Budyanto, L., Y. Goh, and C. Ooi, Fabrication of porous poly (L-lactide)(PLLA) scaffolds for tissue engineering using liquid–liquid phase separation and freeze extraction. Journal of Materials Science: Materials in Medicine, 2009. 20(1): p. 105-111.
- Murphy, S.V. and A. Atala, 3D bioprinting of tissues and organs. Nature biotechnology, 2014. 32(8): p. 773.
- Jang, J., et al., Biomaterials-based 3D cell printing for next-generation therapeutics and diagnostics. Biomaterials, 2018. 156: p. 88-106.
Writer:
Fazilet Gürer
ESR15 - University of Maribor
